Contents
Crohn’s disease
La Crohn’s disease is a chronic inflammatory disease of the digestive system (large intestine), which evolves by openings and phases of remission. It is characterized mainly by crises of abdominal pain and diarrhea, which can last several weeks or several months. Fatigue, weight loss and even undernutrition can occur if no treatment is undertaken. In some cases, non-digestive symptoms, which affect the skin, joints or eyes may be associated with the disease.
How do you recognize the signs of Crohn’s disease?
If you have a Crohn’s disease, the inflammation can affect any part of the digestive tract, from the mouth to the anus. But most often it settles at the junction of thesmall intestine and colon (large intestine).
Crohn’s disease or ulcerative colitis?La Crohn’s disease was first described in 1932 by an American surgeon, the Dr Burril B. Crohn. It is similar in many ways to ulcerative colitis, another common inflammatory bowel disease. To distinguish them, doctors use different criteria. The ulcerative colitis affects only one segment of the digestive tract (= delimited segment of the rectum and colon). For its part, Crohn’s disease can affect other parts of the digestive tract, from the mouth to the intestines (sometimes leaving healthy areas). Sometimes it is not possible to distinguish these two diseases. We then call affection “Indeterminate colitis”. |
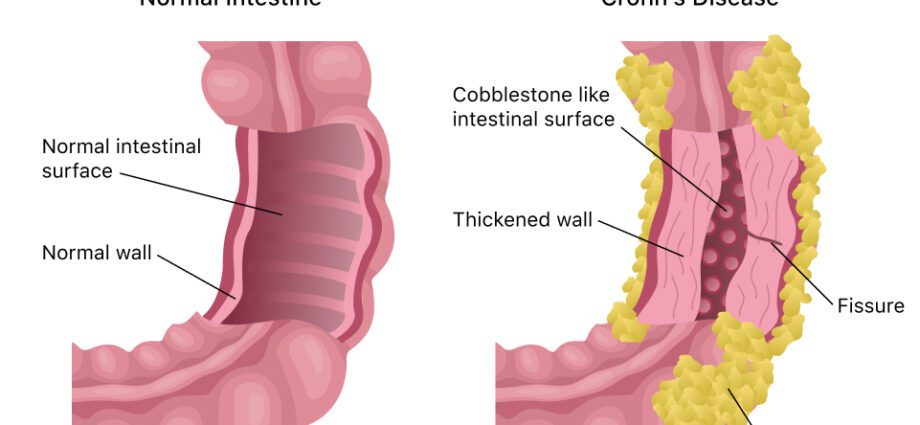
Diagram of Crohn’s disease
What are the causes of Crohn’s disease?
La Crohn’s disease is due to persistent inflammation of the walls and deep layers of the digestive tract. This inflammation can lead to thickening of the walls in some places, cracks and sores in others. The causes of inflammation are unknown and likely multiple, involving genetic, autoimmune and environmental factors.
Genetic factors
Although Crohn’s disease is not a completely genetic disease, certain genes can increase the chances of getting it. In recent years, researchers have discovered several susceptibility genes, including the NOD2 / CARD15 gene, which increases the risk of developing the disease four to five times.6. This gene plays a role in the body’s defense system. However, other factors are necessary for the disease to occur. As in many other diseases, it seems that a genetic predisposition combined with environmental or lifestyle factors triggers the disease.
Autoimmune factors
Like ulcerative colitis, Crohn’s disease has characteristics of an autoimmune disease (= disease where the immune system fights its own cells). Researchers believe that inflammation of the digestive tract is linked to the body’s overreaction of the immune system against viruses or bacteria in the gut.
Environmental factors
It is noted that the incidence of Crohn’s disease is higher in industrialized countries and has tended to increase since 1950. This suggests that environmental factors, probably linked to the Western way of life, could have a significant influence on the onset of the disease. However, no specific factor has yet been identified. Several avenues are however being studied. Exposure to certain antibiotics, especially from the tetracycline class, is a potential risk factor31. Smokers are at greater risk of developing the disease. People who are too sedentary are more affected than people who are more active32.
It is possible, but there is no absolute proof, that a diet too rich in bad fats, meat and sugar increases the risk.33.
The researchers are mainly looking at the possible role of an infection by a virus or a bacterium (salmonella, campylobacter) in triggering the disease. In addition to infection by an “external” microbe, a intestinal flora imbalance (i.e. bacteria naturally present in the digestive tract) could also be involved18.
In addition, certain elements seem to exert a protective effect. These include the diet rich in fiber and fruit, contact before the age of one year with cats or farm animals, appendectomy, as well as having had gastroenteritis or infections. respiratory34. There is also no association between the MMR (measles-rubella-mumps) vaccine and Crohn’s disease.35.
Psychological factors
It has long been thought that stress can trigger seizures. However, studies carried out so far seem to refute this hypothesis.
People at risk
- People with family history inflammatory bowel disease (Crohn’s disease or ulcerative colitis). This would be the case for 10% to 25% of those affected.
- Certain populations are more at risk than others, because of their genetic makeup. The Jewish community (of Ashkenazi origin), for example, would be 4 to 5 times more affected by Crohn’s disease3,4.
How does Crohn’s disease progress?
It is a chronic disease that is present throughout life. Most often the Crohn’s disease evolves in flare-ups interspersed with periods of remission that can last for several months. About 10% to 20% of people have lasting remission after the first outbreak of the disease. The recurrences (or crises) follow one another in a fairly unpredictable way and are of varying intensity. Sometimes the symptoms are so intense (inability to eat, bleeding, diarrhea, etc.) that hospitalization becomes necessary.
Possible complications and consequences
La Crohn’s disease can lead to various health problems. However, the severity of symptoms and complications varies greatly from person to person.
Possible complications
- A obstruction of the digestive tract. Chronic inflammation can cause the lining of the digestive tract to thicken, which can lead to partial or complete blockage of the digestive tract. This can lead to bloating, constipation, or even vomiting of feces. Emergency hospitalization may be necessary to prevent perforation of the intestine.
- Ulcers in the lining of the digestive tract.
- Sores around the anus (fistulas, deep cracks or chronic abscesses).
- Bleeding from the digestive tract, rare but sometimes serious.
- People with Crohn’s disease of the colon have a slightly increased risk of developing colon cancer, especially after several years of the disease, and even if they are in treatment. It is therefore advisable to undergo early and regular screening for colon cancer.
Possible consequences
- A undernutrition, because during crises, patients tend to eat less because of the pain. In addition the ability to absorb food through the wall of the intestine is compromised, in medical language we speak of malabsorption.
- Un growth retardation and puberty in children and adolescents.
- Iron deficiency anemia, due to bleeding in the digestive tract, which can occur in low noise and be invisible to the naked eye.
- Other health problems, such as arthritis, skin conditions, inflammation of the eyes, mouth ulcers, kidney stones or gallstones.
- Crohn’s disease, when in the “active” phase, increases the risk ofspontaneous abortion in pregnant women who have it. It can make it difficult for the fetus to grow. It is therefore important that women who wish to become pregnant control their disease very well with the help of treatments and discuss it with their doctor.
How many people are affected by Crohn’s disease?
According to the Afa website, it is in Northwest Europe and the United States that we find the most people affected by Crohn’s disease. In France, around 120.000 people are said to be affected. In these regions, the Afa counts 4 to 5 cases per 100.000 inhabitants each year.
In Canada, the Crohn’s disease affects about 50 people per 100 population in industrialized countries, but there is great variability by geographic region. The place in the world with the most reported cases is in Nova Scotia, a Canadian province, where the rate climbs to 000 per 319 people. In Japan, Romania and South Korea, the rate is less than 100,000 per 2529.
The disease can occur at any age, including childhood. It is usually diagnosed in people 10 to 30 years old30.
Our doctor’s opinion on the disease
As part of its quality approach, Passeportsanté.net invites you to discover the opinion of a health professional. Dr Dominic Larose, emergency physician gives you his opinion on the Crohn’s disease :
Crohn’s disease is a disease that usually will follow you for life. Understanding this disease and its treatments can provide an excellent quality of life for the majority of affected patients. This disease evolves into flare-ups and remissions. It is therefore necessary to be wary of the fortuitous associations which you can make. If you have more pain on a Tuesday morning, it doesn’t necessarily have to do with what you ate on Monday evening. And if you are feeling better, it is not necessarily because of the homeopathic granules you took the day before. It is only with randomized double-blind research that it can be said that a treatment may or may not be effective. Stay vigilant, avoid miracle cures, have an excellent hygiene of life, and find a doctor who will follow you closely. Joint follow-up with a gastroenterologist is strongly suggested. We can live well with the disease! Dominic Larose MD CMFC(MU) FACEP, urgentiste |